Welches Risiko birgt eine SARS-CoV-2-Infektion für Mütter und ihr ungeborenes Kind? Sollten sich Schwangere gegen das Virus impfen lassen? Unsere Expert:innen Dr. Cathrin Kodde und Prof. Dr. Michael Friedrich geben Antworten.
Die Geburt eines Kindes ist für werdende Eltern etwas ganz Besonderes. Sie gehört zu den schönsten und eindrücklichsten Erfahrungen im Leben. Doch das Coronavirus stellt Schwangere und Geburtsstationen vor neue Herausforderungen. Wir haben zusammengefasst, was werdende Eltern wissen müssen.
Etwa jede zehnte Schwangere leidet unter Bluthochdruck. Nur in seltenen Fällen ist ein erhöhter Blutdruck ein Anzeichen für eine Präeklampsie, umgangssprachlich auch als „Schwangerschaftsvergiftung“ bezeichnet. Hier erfahren Sie mehr über Bluthochdruck in der Schwangerschaft und wann es sich um eine Präeklampsie handelt.
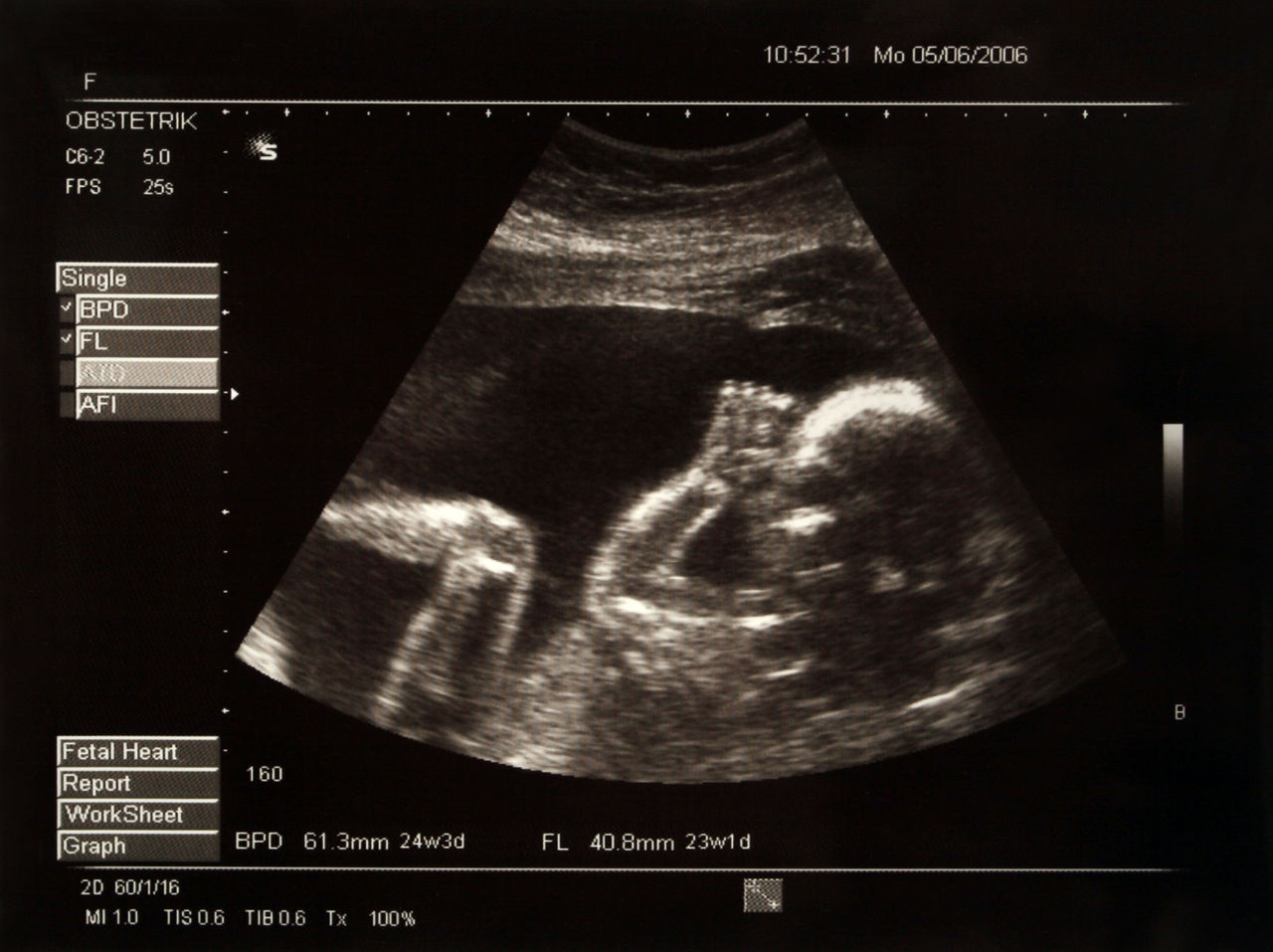
Während der Schwangerschaft werden zahlreiche Untersuchungen angeboten, um die Entwicklung des ungeborenen Kindes zu beurteilen. Da können werdende Eltern schnell den Überblick verlieren. Welche Untersuchungen wirklich wichtig sind, erklären wir Ihnen hier.
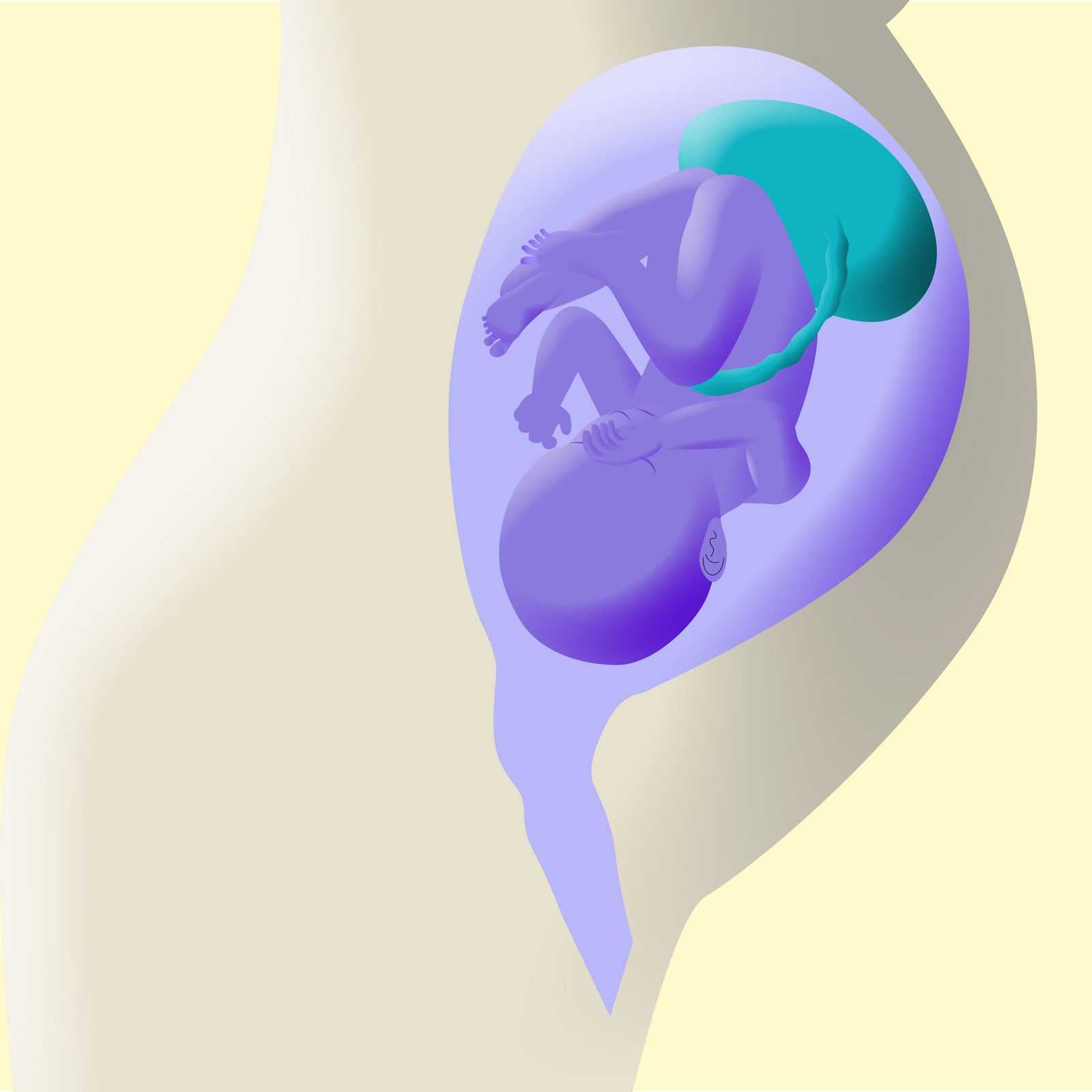
In 40 Schwangerschaftswochen wächst nicht nur das Baby, sondern auch die Plazenta. Was der Mutterkuchen tatsächlich leistet in dieser Zeit, welche Aufgaben und Funktionen die Plazenta übernimmt, erklärt unser Experte.
Sie leiden an Rheuma und möchten schwanger werden? In der Regel steht mit dieser chronischen Erkrankung dem Kinderwunsch nichts im Wege. Was Sie bei Rheuma in der Schwangerschaft beachten müssen, lesen Sie hier.
Oft fragen sich werdende Mütter, ob Reisen in der Schwangerschaft möglich ist. Die Antwort ist ganz einfach: Ja. Allerdings sollten einige Dinge bei der Planung und Durchführung der Reise beachtet werden. Wir haben einige Tipps für Sie zusammengestellt.
Jeder dritte Erwachsene in Deutschland hat Veränderungen an der Schilddrüse – viele, ohne es zu wissen. Und so klein das schmetterlingsförmige Organ auch ist, sein Einfluss ist groß. Gerade in der Schwangerschaft können Funktionsstörungen der Schilddrüse für die werdende Mutter und ihr ungeborenes Kind gravierende Folgen nach sich ziehen. Unser Experte erläutert, worauf Schwangere achten sollten.
Mit der Schwangerschaft beginnt für Frauen eine aufregende Zeit – voller Vorfreude, aber auch voller Veränderungen. Erfahren Sie, wie sich das Baby in den 40 Schwangerschaftswochen bis zur Geburt entwickelt, was im Körper der werdenden Mutter passiert und worauf Sie bei Ernährung und Alltagstätigkeiten achten sollten.

Mom2B – der Schwangerschaftspodcast
Kinderwunsch, Fruchtbarkeit, Entwicklung des Babys, Dos und Don'ts in der Schwangerschaft: Rund um die Schwangerschaft gibt es viel zu wissen. Unsere Podcastreihe Mom2B – bestens beraten durch die Schwangerschaft ist Ihr Begleiter durch eine aufregende Zeit. Hören Sie mal rein!
Das Coronavirus wirft viele Fragen und Unsicherheiten auf – gerade auch bei Schwangeren und Stillenden. Die Deutsche Gesellschaft für Gynäkologie und Geburtshilfe e. V. (abgekürzt DGGG) gibt Antworten auf häufig gestellte Fragen, die wir hier für Sie auf einen Blick zusammengefasst haben (Stand 2020).
Etwa jede zehnte Schwangere leidet unter Bluthochdruck. Nur in seltenen Fällen ist ein erhöhter Blutdruck ein Anzeichen für eine Präeklampsie, umgangssprachlich auch als „Schwangerschaftsvergiftung“ bezeichnet. Hier erfahren Sie mehr über Bluthochdruck in der Schwangerschaft und wann es sich um eine Präeklampsie handelt.
Sie leiden an Rheuma und möchten schwanger werden? In der Regel steht mit dieser chronischen Erkrankung dem Kinderwunsch nichts im Wege. Was Sie bei Rheuma in der Schwangerschaft beachten müssen, lesen Sie hier.
Jeder dritte Erwachsene in Deutschland hat Veränderungen an der Schilddrüse – viele, ohne es zu wissen. Und so klein das schmetterlingsförmige Organ auch ist, sein Einfluss ist groß. Gerade in der Schwangerschaft können Funktionsstörungen der Schilddrüse für die werdende Mutter und ihr ungeborenes Kind gravierende Folgen nach sich ziehen. Unser Experte erläutert, worauf Schwangere achten sollten.
Während einer Schwangerschaft sowie nach einer Geburt fahren die Gefühle vieler Frauen Achterbahn: Glücksmomente wechseln sich mit Traurigkeit und Erschöpfung ab. Das ist normal und auf die hormonellen Umstellungen des Körpers zurückzuführen. Wenn die negativen Gefühle jedoch übermächtig werden, kann das ein Hinweis auf eine Schwangerschaftsdepression sein.
Der Schwangerschaftsdiabetes (in Fachkreisen Gestationsdiabetes mellitus) gilt als die häufigste Begleiterkrankung einer Schwangerschaft und kann unbehandelt zu ernsten Komplikationen für Mutter und Kind führen. Hier erfahren Sie alles Wissenswerte rund um Symptome, Folgen und Prävention.
Die Geburt eines Kindes sollte eine der schönsten Erfahrungen sein. Die Hormone spielen verrückt. Eltern spüren Freude, Glück und eine unfassbare Liebe. Doch dieses Erlebnis kann auch negative Gefühle, wie Hilflosigkeit oder Angst, hervorrufen. Einige Mütter entwickeln in der Zeit danach, dem Wochenbett, eine Wochenbettdepression.
Sie leiden an Epilepsie und möchten schwanger werden? In der Regel steht mit dieser chronischen Erkrankung dem Kinderwunsch nichts im Wege. Was Sie bei Epilepsie in der Schwangerschaft beachten müssen, lesen Sie hier.
Sie haben Asthma und möchten schwanger werden? In der Regel steht mit dieser chronischen Erkrankung dem Kinderwunsch nichts im Wege. Was Sie bei Asthma in der Schwangerschaft beachten müssen, lesen Sie hier.
Mammakarzinom: Diese Diagnose erhalten in Deutschland rund 70.000 Frauen pro Jahr. Damit ist Brustkrebs – so der gängige Name – die häufigste Krebserkrankung bei Frauen. Besonders belastend ist die Diagnose Brustkrebs in der Schwangerschaft.
Endometriose kann jede Frau treffen: vom Eintritt der Regelblutung bis zu den Wechseljahren. Pro Jahr erkranken in Deutschland etwa acht bis 15 Prozent von ihnen an dieser Wucherung der Gebärmutterschleimhaut. Was dies für Kinderwunsch oder Schwangerschaft bedeutet, lesen Sie hier.
Eine Frühgeburt wird definiert als Geburt vor der abgeschlossenen 37. Schwangerschaftswoche (SSW). Deutschland hat eine der höchsten Frühgeburtenraten in Europa. Dabei können die Risikofaktoren gut beeinflusst werden. Wir zeigen Ihnen, wie Sie Infektionen, die häufigsten Auslöser für eine Frühgeburt, in der Schwangerschaft verhindern können?
Manche Infektionskrankheiten in der Schwangerschaft verlaufen für die Mutter harmlos, bleiben sogar meistens unbemerkt, während sie gleichzeitig für das ungeborene Kind sehr gefährlich werden können. Warum ist das so?
Sie leiden an Multipler Sklerose, kurz MS, und möchten schwanger werden? In der Regel steht mit dieser chronischen Erkrankung dem Kinderwunsch nichts im Wege. Was Sie bei MS in der Schwangerschaft beachten müssen, lesen Sie hier.
Sie leiden an Neurodermitis und möchten schwanger werden? In der Regel steht mit dieser chronischen Erkrankung dem Kinderwunsch nichts im Wege. Was Sie bei Neurodermitis in der Schwangerschaft beachten müssen, lesen Sie hier.
Die Omphalozele ist eine angeborene Fehlbildung. Sie lässt sich bereits früh in der Schwangerschaft diagnostizieren. Erfahren Sie, was dies für das Neugeborene und werdende Eltern bedeutet.
Wassergeburten werden immer beliebter. Das Baby im warmen Wasser zur Welt zu bringen, kann entspannend und schonend sein. Was sind die Vorteile? Worauf muss ich achten? Das lesen Sie hier.
Stillen bereitet vielen Neu-Mamas Schwierigkeiten und Falschinformationen verunsichern zusätzlich. Expertin Ute Voß, Still- und Laktationsberaterin des Mutter-Kind-Zentrums am Helios Klinikum Krefeld, räumt mit den häufigsten Still-Mythen auf und gibt hilfreiche Tipps.
Oft fragen sich werdende Mütter, ob Reisen in der Schwangerschaft möglich ist. Die Antwort ist ganz einfach: Ja. Allerdings sollten einige Dinge bei der Planung und Durchführung der Reise beachtet werden. Wir haben einige Tipps für Sie zusammengestellt.
Mit der Schwangerschaft beginnt für Frauen eine aufregende Zeit – voller Vorfreude, aber auch voller Veränderungen. Erfahren Sie, wie sich das Baby in den 40 Schwangerschaftswochen bis zur Geburt entwickelt, was im Körper der werdenden Mutter passiert und worauf Sie bei Ernährung und Alltagstätigkeiten achten sollten.
„Ist der Bauch spitz, wird es ein Junge.“ Oder: „Einmal Kaiserschnitt, immer Kaiserschnitt“. Wer kennt sie nicht, die kuriosen Mythen rund um Schwangerschaft und Geburt? Von Generation zu Generation weitererzählt, halten sie sich hartnäckig. Was ist dran an diesen Schwangerschaftsmythen? Hebamme Yvonne Schildai klärt auf.
Wenn die Temperaturen im Sommer nach oben klettern, kann es für Schwangere anstrengend werden. Der Alltag mit Babybauch ist in der Hitze eine echte Herausforderung – ganz gleich in welcher Phase der Schwangerschaft. Mit den Tipps unserer Expertin haben es Schwangere im Sommer leichter.
Galt eine Schwangerschaft jenseits der 30 früher noch als Ausnahme, ist spätes Mutterglück heute ganz normal. Je älter die Frau, desto schwieriger wird es allerdings mit dem Kinderkriegen. Schwanger mit 40 – hier erfahren Sie, wie es trotzdem klappen kann.
Werdende Mütter möchten alles richtig machen – und vor allem ihrem Baby nicht durch falsches Verhalten schaden. Viele fragen sich deshalb, ob Sport in der Schwangerschaft für ihr Ungeborenes gefährlich sein könnte. In der Regel nicht, sofern einige Dinge berücksichtigt werden.
Schon zu Beginn der Schwangerschaft stellen sich viele werdende Mütter die Frage: Soll ich meinem Kind die Brust geben oder doch eher auf die Flasche zurückgreifen? Hier lesen Sie, worauf Sie bei der Ernährung Ihres Babys in den ersten Wochen und Monaten achten sollten.
Bevor ein Baby das Licht der Welt erblickt, gibt es für die werdenden Eltern viel zu organisieren und zahlreiche Fragen zu beantworten: In welcher Klinik soll das Kind geboren werden? Und wann muss ich mich dort anmelden? Welche Unterlagen brauche ich? Wir beantworten diese und andere Fragen, die vor der Geburt wichtig sind.
Etwa jede dritte Schwangere spürt Wochen vor dem Geburtstermin vereinzelt Wehen. Oft handelt es sich dabei um Übungswehen. Doch wie erkennen Schwangere, ob alles gut ist oder sie besser ärztlichen Rat einholen sollten? Hier erfahren Sie es.
Wie soll mein Neugeborenes schlafen, wie trage ich es richtig und welche Kleidung ist am besten? Eltern wollen keine Fehler im Umgang mit ihren Babys machen. Unsere Expertin gibt Tipps, wie Sie mit Ihrem Neugeborenen richtig umgehen.
Haarausfall, Müdigkeit oder Kopfschmerzen können Anzeichen für einen Mangel an Vitamin D sein. Viele Frauen sind von einem solchen Vitamin-D-Mangel in der Schwangerschaft betroffen. Ob eine vorsorgliche Einnahme von Vitamin-D-Präparaten notwendig ist, erklärt Krzysztof Szkaradzinski, Chefarzt für Gynäkologie und Geburtshilfe am Helios Vogtland-Klinikum Plauen.
Die Geburt ist geschafft. Ihr Körper hat Schwerstarbeit geleistet und nun erholt er sich langsam wieder. Ungefähr sechs bis acht Wochen nach der Geburt dauert das Wochenbett. Welche körperlichen Umstellungen Sie erwarten, wie Sie Beschwerden lindern können und worauf Sie achten sollten, haben wir hier zusammengestellt.
Kleidung, Dokumente, Nervennahrung: Sie stehen kurz vor der Geburt und haben noch keine Kliniktasche gepackt? Lesen Sie hier, was Sie für die Geburt und die Tage danach in der Klinik brauchen.
Die Zeit nach der Geburt ist geprägt von Veränderungen und vielen Fragen. Sobald Sie mit Ihrem Kind zu Hause sind, beginnt die Wochenbettbetreuung durch eine Hebamme. Hier erfahren Sie mehr.
Je näher der errechnete Geburtstermin rückt, desto mehr kreisen die Gedanken um den Geburtsbeginn: Vor allem die Frage „Wann muss ich in die Klinik fahren?“ beschäftigt viele Frauen. Welche klaren Zeichen es gibt, lesen Sie hier.
Das Baby ist da und wird auf den nackten Oberkörper der Mutter oder des Vaters gelegt. Diese erste direkte Kontaktaufnahme, dieses erste Beschnuppern und Spüren der Eltern baut Vertrauen und Geborgenheit auf. Der Fachbegriff dafür ist Bonding. Hier erfahren Sie mehr.
Verläuft eine Schwangerschaft komplikationslos, können werdende Eltern nach den eigenen Bedürfnissen entscheiden, wie und wo sie entbinden möchten. Hier gibt es verschiedene Wahlmöglichkeiten. Eine gute Vorbereitung und Information ist dabei sehr hilfreich.
40 Wochen keinen Camembert, kein Sushi, keine Salami. Werdende Mütter sind zu Beginn der Schwangerschaft plötzlich vor neue Regeln zur richtigen Ernährung gestellt. Doch was heißt das genau und warum sind manche Empfehlungen so streng? Hier lesen Sie mehr.
Gerade bei der ersten Schwangerschaft haben Frauen jede Menge Fragen rund um das Thema Geburt. Wir beantworten die wichtigsten Fragen.
Die Zeit kurz vor dem Geburtstermin ist für Sie als werdende Mama besonders aufregend. Sie stellen sich sicher häufig die Frage, wann sich Ihr Sprössling endlich auf den Weg macht? Die Antwort ist simpel: Ihr Baby kommt, wenn der richtige Zeitpunkt da ist. Hebamme Corinna Erlinger aus der Helios Klinik in Bad Saarow gibt Tipps für natürliche Mittel und Wege, die Wehen fördern können.
Unsere Kreißsäle bieten alle Voraussetzungen für verschiedenste Geburtspositionen. Wir unterstützen Sie bei der Wahl Ihrer Geburtsposition und geben Ihnen und auch Ihrem Partner Hilfestellung, damit die Geburt ein schönes Erlebnis wird.
Schwangere mussten sich entscheiden: Entweder für eine Geburt zu Hause, im Geburtshaus in Begleitung einer Hebamme oder für eine Geburt im ärztlich geleiteten Kreißsaal eines Krankenhauses. Mit dem Hebammenkreißsaal gibt es eine Alternative. Wie funktioniert sie?
Das Mutterschutzgesetz schützt schwangere Frauen und ihre ungeborenen Kinder vor und auch nach der Geburt so gut wie möglich. Was werdende Mütter und ihre Arbeitgeber:innen wissen und beachten sollten, lesen Sie hier.
Das Baby ist da. Und was kommt dann? Was erwartet Mutter und Kind in der Klinik oder zu Hause? Hier erfahren Sie, wie es für Sie und Ihr Kind nach der Entbindung im Kreißsaal weitergeht.
Die Geburt – ein natürlicher Vorgang. Besetzt mit Vorfreude, Ängsten und Erwartungen. An dieser Stelle möchten wir Ihnen einen kleinen Einblick in den Ablauf einer natürlichen Geburt und in die Abläufe in einem Kreißsaal geben.
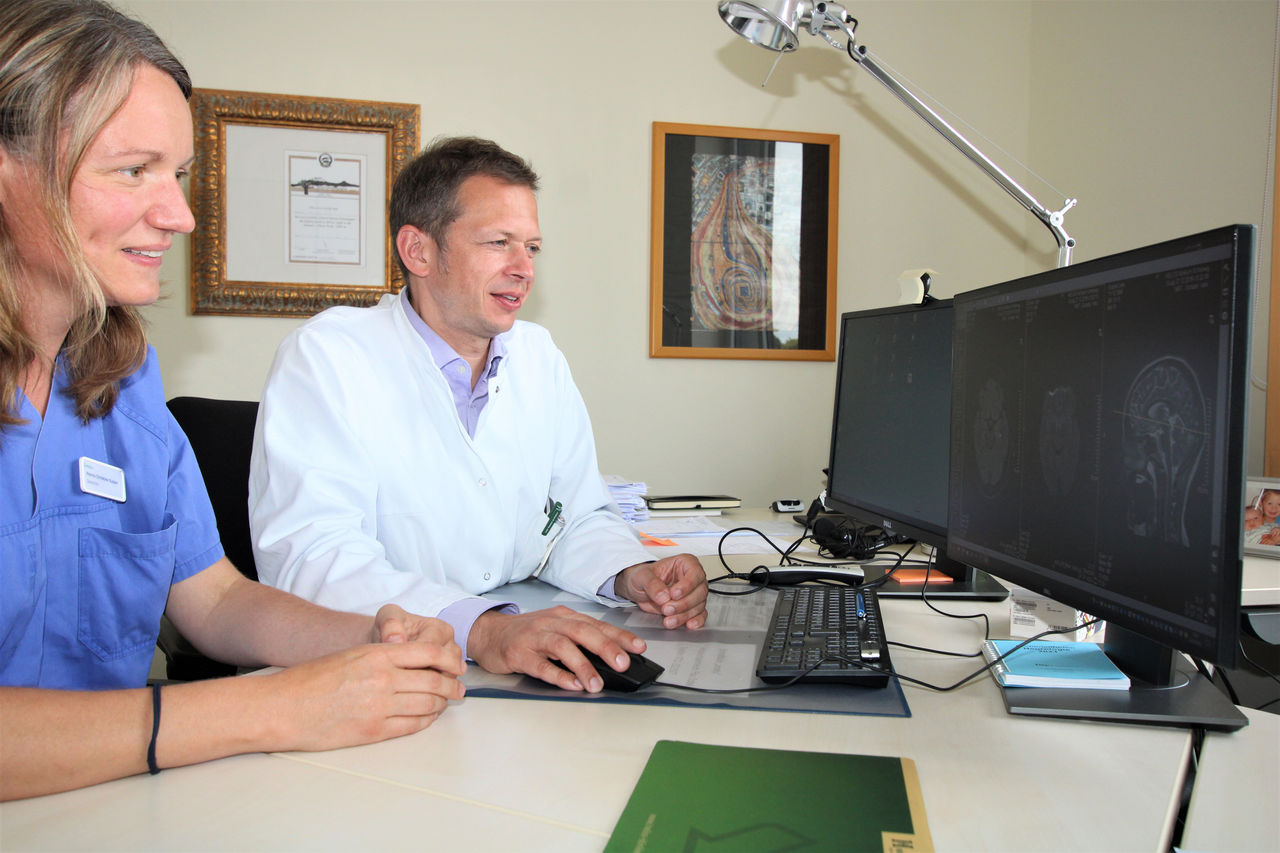
Finden Sie den richtigen Ansprechpartner ganz in Ihrer Nähe in einer unserer Kliniken, Zentren, Arztpraxen oder Spezialkliniken. Geben Sie die Postleitzahl und den gewünschten Umkreis zu Ihrem Thema ein und wählen Sie die passende Einrichtung.
Sie haben noch nicht das passende Angebot gefunden? Dann rufen Sie uns einfach an unter: (0800) 8 123 456
Während der Schwangerschaft werden zahlreiche Untersuchungen angeboten, um die Entwicklung des ungeborenen Kindes zu beurteilen. Da können werdende Eltern schnell den Überblick verlieren. Welche Untersuchungen wirklich wichtig sind, erklären wir Ihnen hier.
Die Zahl der Kinderwunschbehandlungen steigt, denn etwa jedes sechste Paar ist ungewollt kinderlos. Wurden im Jahr 1997 noch gut 6.500 Kinder nach einer Kinderwunschbehandlung geboren, sind es im Jahr 2020 bereits über 22.200. Was Paare mit Kinderwunsch über die künstliche Befruchtung wissen sollten, lesen Sie hier.
Geburtsschmerzen können unterschiedlich stark empfunden werden. Es gibt eine Auswahl verschiedener Therapien – von klassischen Schmerzmitteln bis zu naturheilkundlichen Verfahren, die den Schmerz lindern. Lesen Sie hier mehr dazu.
Wassergeburten werden immer beliebter. Das Baby im warmen Wasser zur Welt zu bringen, kann entspannend und schonend sein. Was sind die Vorteile? Worauf muss ich achten? Das lesen Sie hier.
Egal, ob geplant oder nicht geplant: Ein Kaiserschnitt ist ein größerer operativer Eingriff in Vollnarkose oder Regionalanästhesie, der bis zu 60 Minuten dauern kann. Welche Arten von Kaiserschnitt gibt es und was gilt es zu beachten?
Stillen ist die natürlichste Art ein Kind ausgewogen zu ernähren, optimal zu schützen und ihm von Anfang an Geborgenheit zu bieten. Doch viele Frauen machen gerade zu Beginn der Stillzeit die schmerzhafte Erfahrung wunder oder entzündeter Brustwarzen. Wie die Low Level Laser Therapie hilft, lesen Sie hier.
Unter der Geburt kommt es zu Schmerzen, wo sich Schwangere eine schnelle Linderung wünschen. Hier stehen verschiedene alternative Behandlungsmethoden zur Verfügung. Dazu zählen etwa Akupunktur, Homöopathie, Hypnose und Kinesiologie. Was verbirgt sich dahinter?
Fünf Prozent aller Kinder liegen vor dem Geburtstermin mit dem Gesäß voran im Beckenausgang der Mutter. Diese Beckenendlage erschwert einen natürlichen Geburtsverlauf für Mutter und Kind. Ist eine normale Geburt so überhaupt möglich? Lesen Sie hier den Erfahrungsbericht von Rosalia W.
Etwa die Hälfte aller Frauen in Deutschland ist übergewichtig. Bei einer Schwangerschaft können zusätzliche Kilos zu ernstzunehmenden Komplikationen führen. Schwangere können die Risiken allerdings selbst positiv beeinflussen. Unser Experte erklärt alles Wissenswerte dazu.
Moderne Medikamente, hochspezialisierte Narkoseärzt:innen und modernste technische Ausstattung gewährleisten eine sichere Narkose. Erfahren Sie hier mehr über den Fachbereich der Anästhesiologie.
Bei circa fünf Prozent aller Geburten liegt das Baby am Ende der Schwangerschaft in Beckenendlage. Die sogenannte Steißlage führt oft zum Kaiserschnitt, aber unter bestimmten Voraussetzungen ist auch eine natürliche Geburt möglich. Doch wie kommt es zur Beckenendlage und was sollten Schwangere wissen? Unsere Expertin klärt auf.
Bei Rabia Araci droht eine Frühgeburt in der 23. Schwangerschaftswoche. Die Chancen für ihre Tochter stehen nicht gut, die Kleine wiegt gerade einmal rund 600 Gramm. Acht Wochen lang kämpft die werdende Mama im Kreißsaal der Helios St. Johannes Klinik in Duisburg mit Hilfe des Teams um jeden Tag.
In Deutschland kommt es jährlich zu rund 60.000 Frühgeburten, davon ungefähr 8.000 mit einem Gewicht von unter 1.500 Gramm. Diese sehr kleinen Frühchen und andere kranke Neugeborene bedürfen besonderer, hoch qualifizierter Pflege und medizinischer Versorgung. Mehr dazu lesen Sie hier.
Eine normalverlaufende Schwangerschaft dauert etwa 40 Wochen und endet mit dem Blasensprung, dem Einsetzen der Wehen und der Geburt des Kindes – so die Theorie. Was aber, wenn Komplikationen auftreten oder nach der 40. Schwangerschaftswoche keine Wehen einsetzen? Dann müssen Ärzt:innen die Geburt einleiten.
Die geburtsvorbereitende Akupunktur zum Ende der Schwangerschaft hat sich in den letzten Jahren immer mehr etabliert. So kann sie Geburtsschmerzen reduzieren und die Geburt erleichtern. Doch wie funktioniert das genau? Cindy Spichal, Leitende Hebamme in der Helios St. Marienberg Klinik Helmstedt, gibt Auskunft.
Schwangere mussten sich entscheiden: Entweder für eine Geburt zu Hause, im Geburtshaus in Begleitung einer Hebamme oder für eine Geburt im ärztlich geleiteten Kreißsaal eines Krankenhauses. Mit dem Hebammenkreißsaal gibt es eine Alternative. Wie funktioniert sie?
Viele werdende Mütter haben ein mulmiges Gefühl, wenn es langsam aber sicher in Richtung Geburt geht. Schauergeschichten aus dem Freundes- und Bekanntenkreis oder auch die Angst vor Schmerzen führen nicht selten zu Verunsicherung. Muss die natürliche Geburt zwingend schmerzhaft oder traumatisch sein? Wir erläutern das Konzept Hypnobirthing.
Jedes zehnte Paar in Deutschland ist ungewollt kinderlos. Für Betroffene ist der unerfüllte Kinderwunsch oft mit Scham und Schuldgefühlen behaftet. Doch die moderne Medizin kann helfen. Wir informieren Sie hier über die möglichen Ursachen von Unfruchtbarkeit und Infertilität und erklären, welche Behandlungsmöglichkeiten es gibt.
Filos Geburt ist das größte Geschenk für Dunia M.* und ihren Mann. Das vierte Kind sollte wie die drei älteren Geschwister per Kaiserschnitt zur Welt kommen. Doch in den Voruntersuchungen zeigte sich, dass dieser Eingriff ein lebensbedrohliches Risiko für Mutter und Kind sein würde.
In den letzten Monaten einer Schwangerschaft rückt der lang ersehnte Tag der Geburt immer näher. Dabei spielt eine entscheidende Frage eine große Rolle: Wie soll das Kind auf die Welt kommen? Unser Experte Thomas Köster erklärt alles Wissenswerte über beide Geburtsformen.
Ungewollte Kinderlosigkeit betrifft in Deutschland rund jedes zehnte Paar mit Kinderwunsch. Welche Möglichkeiten bietet die künstliche Befruchtung? Wie hoch sind die Erfolgschancen? Und: Wer übernimmt die Kosten? Diese Fragen beantworten hier unsere Experten.
Eine gute Alternative zur Periduralanästhesie (PDA) bei der Geburt ist das sogenannte Lachgas. Es lindert die Schmerzen, ohne das Geburtserlebnis zu mindern und kann auch zu einem späteren Zeitpunkt noch angewendet werden. Hier erfahren Sie mehr.
Die Geburt eines Kindes ist für werdende Eltern Glück und Herausforderung zugleich. Wenn es sich dann noch um Zwillinge oder gar Drillinge handelt, ist die erste Zeit nach der Entbindung meist besonders intensiv. Lesen Sie hier alles über Mehrlingsschwangerschaften.
Misgav Ladach – der sanfte Kaiserschnitt – ermöglicht trotz Operation ein bewussteres Geburtserlebnis als bei einem herkömmlichen Kaiserschnitt und ist besonders schonend für die Mutter. Lesen Sie hier, worum es geht.
Die Geburt – ein natürlicher Vorgang. Besetzt mit Vorfreude, Ängsten und Erwartungen. An dieser Stelle möchten wir Ihnen einen kleinen Einblick in den Ablauf einer natürlichen Geburt und in die Abläufe in einem Kreißsaal geben.
Welches Risiko birgt eine SARS-CoV-2-Infektion für Mütter und ihr ungeborenes Kind? Sollten sich Schwangere gegen das Virus impfen lassen? Unsere Expert:innen Dr. Cathrin Kodde und Prof. Dr. Michael Friedrich geben Antworten.
Die aktuelle Corona-Situation ist für die meisten von uns belastend. Vor allem werdende Eltern stehen mitten in der Pandemie vor einer ganz besonderen Herausforderung: In das ungewohnte Gefühlschaos mischen sich auch Sorgen darüber, wie die Schwangerschaft und anschließende Geburt unter den Corona-Bedingungen ablaufen werden. Maria Lopez, leitende Hebamme, und Dr. Kerstin Hammer, Leiterin der Geburtshilfe und Pränatalmedizin in der Helios Mariahilf Klinik in Hamburg räumen mit sieben weitverbreiteten Irrtümern zum Thema Schwangerschaft und Geburt während der Pandemie auf.
Die Geburt eines Kindes ist für werdende Eltern etwas ganz Besonderes. Sie gehört zu den schönsten und eindrücklichsten Erfahrungen im Leben. Doch das Coronavirus stellt Schwangere und Geburtsstationen vor neue Herausforderungen. Wir haben zusammengefasst, was werdende Eltern wissen müssen.
Galt eine Schwangerschaft jenseits der 30 früher noch als Ausnahme, ist spätes Mutterglück heute ganz normal. Je älter die Frau, desto schwieriger wird es allerdings mit dem Kinderkriegen. Schwanger mit 40 – hier erfahren Sie, wie es trotzdem klappen kann.
Vermutlich würden Sie am liebsten jetzt schon Ihr Baby in den Armen halten, aber es muss erst einmal in Ihrem Bauch heranwachsen. Welche rasanten Entwicklungsschritte es dabei in den 40. Schwangerschaftswochen macht und welche kleinen Wunder in Ihrem Bauch passieren, erfahren Sie hier.
Das zweite Trimester ist für werdende Eltern besonders spannend. Das Baby entwickelt sich in rasantem Tempo: Die Geschlechtsteile bilden sich aus und es öffnet zum ersten Mal seine Augen. Viele Frauen empfinden diese Phase der Schwangerschaft am angenehmsten.
Bis das Baby zur Welt kommt, hat die Fruchtblase eine wichtige Funktion: Sie umschließt den Fötus und das Fruchtwasser, wächst mit ihm und schützt ihn – bis zur Geburt. Manchmal kommt es allerdings zu einem vorzeitigen Blasensprung – was passiert dann? Hier erfahren Sie mehr.
Drillingsgeburten sind ein großes Ereignis: Sie sind nicht nur selten, sondern auch die Drillingsschwangerschaft stellt werdende Mütter vor ziemliche Herausforderungen.
Naht der Geburtstermin, werden viele werdende Mütter unsicher oder sogar ängstlich. Das Wissen um den normalen Ablauf einer Geburt kann helfen, eventuelle Ängste vor dem Ungewissen abzubauen. Hier lesen Sie mehr.
Egal in welchem Stadium einer Schwangerschaft, Fehlgeburten sind für die Familien und vor allem für die Frauen sehr belastend. Eine Missed Abortion ist eine sogenannte „verhaltene“ Fehlgeburt – es kommen plötzlich keine Lebenszeichen mehr vom Kind. Mehr dazu lesen Sie hier.
Es begann mit hämmernden Kopfschmerzen – und endete mit einem achtmonatigen Krankenhausaufenthalt. Eine Autoimmunerkrankung riss die damals schwangere Jana Grigoleit mitten aus dem Leben. Ein Fall, der auch für die Mediziner:innen im Helios Klinikum Schleswig einzigartig ist.
Bei Rabia Araci droht eine Frühgeburt in der 23. Schwangerschaftswoche. Die Chancen für ihre Tochter stehen nicht gut, die Kleine wiegt gerade einmal rund 600 Gramm. Acht Wochen lang kämpft die werdende Mama im Kreißsaal der Helios St. Johannes Klinik in Duisburg mit Hilfe des Teams um jeden Tag.
In Lea schlummern schon immer zwei große Interessensfelder: Das Kreative mit Kultur und Musik und das Soziale. Nach der Geburt ihres Sohnes Joona im April 2018 steht für Lea Zerbe (28) fest: „Das Soziale überwiegt. Ich will Hebamme werden!“ Lesen Sie hier ihren Bericht.


.jpg/_jcr_content/renditions/cq5dam.web.1280.1280.jpeg)