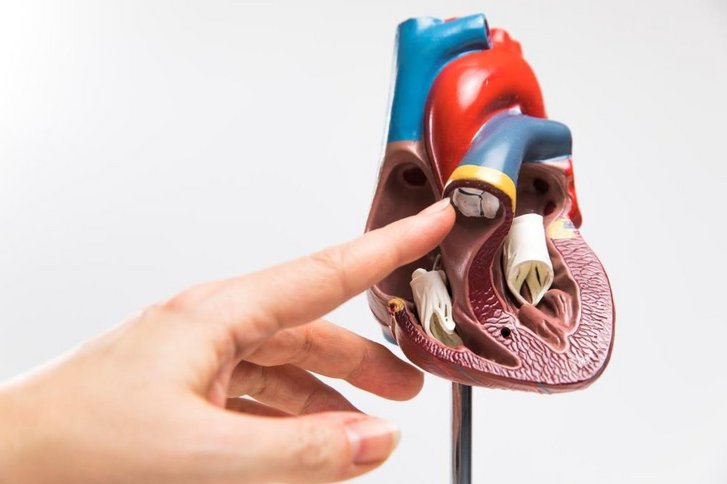
The aortic valve connects the left ventricle of the heart to the aorta, the main artery in the human body. It has three leaflets, which open as the heart contracts and close after each contraction to prevent blood from flowing back from the aorta to the heart. Aortic valve surgery is performed to treat an aortic valve which has narrowed (aortic valve stenosis) or is leaking (aortic valve insufficiency).
